Chronic back pain is extremely common, with up to 80% of adults experiencing lower back pain in their lifetime, and lower back pain being the single leading cause of disability in the world (WHO, 2023). It deeply affects a person’s quality of life. Photobiomodulation is emerging as a supportive option for many types of pain, and this case highlights how consistent treatment can create meaningful change—even when hope feels low.
A woman in her 50s presented with chronic lower back pain that was most severe in the mornings, rating it at 8/10. She had undergone multiple back surgeries, including a spinal fusion, which helped her regain mobility but did not resolve her ongoing pain. Her symptoms continued to interfere with her sleep and daily activities.
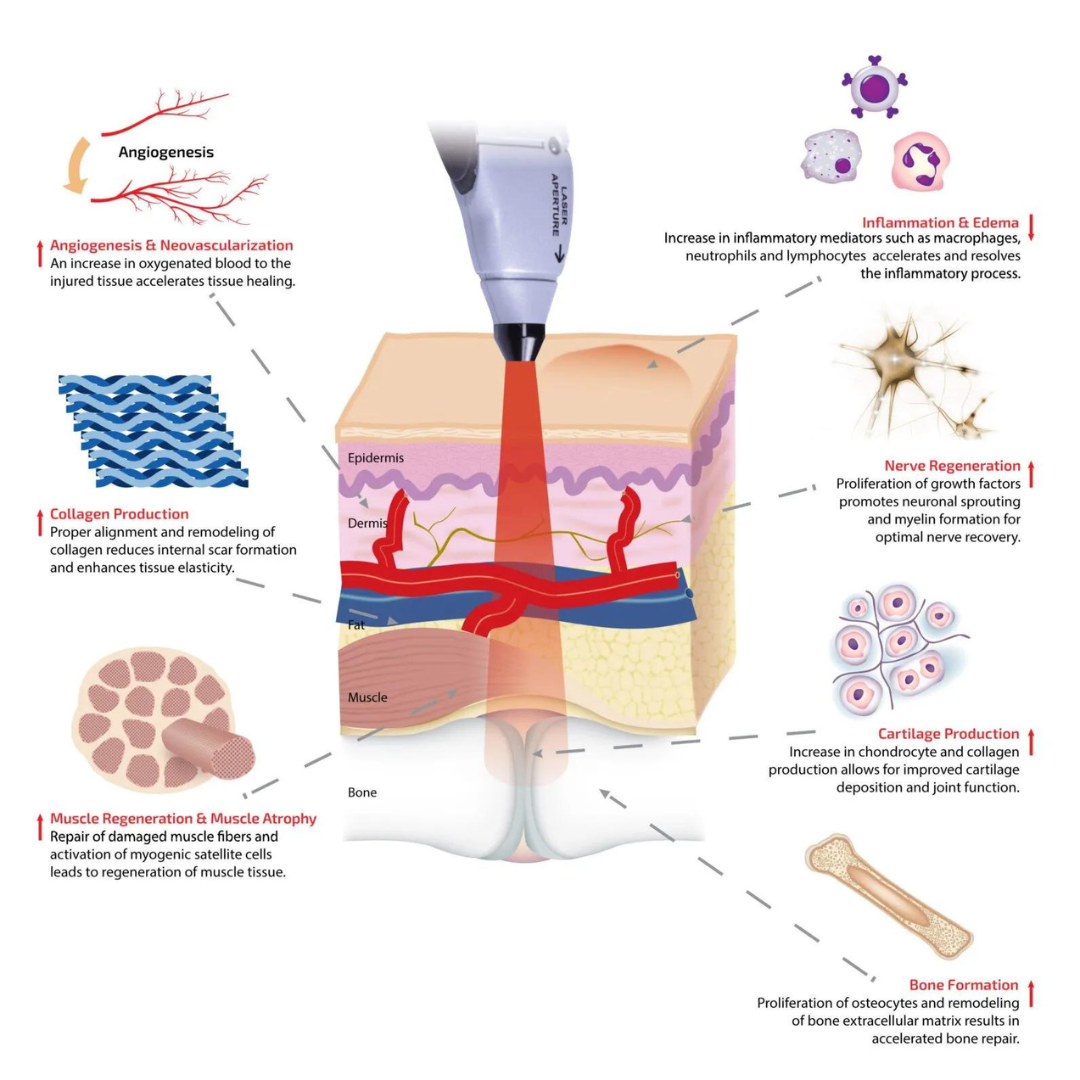
Photobiomodulation is a non-invasive therapy that uses specific wavelengths of light—such as red LED, infrared, and cold laser—to decrease pain, reduce inflammation, improve circulation, and support joint healing. Because of the severity of her symptoms, we began with photobiomodulation sessions twice per week for the first four treatments, then gradually spaced them out based on her progress. She was also receiving osteopathic manual therapy concurrently.
At her first visit, her pain was rated at 8/10. Following the initial photobiomodulation session, I recommended joint-supportive and anti-inflammatory supplementation. By her third treatment, her pain had decreased to 4/10, and she noted improvements in her sleep. We also discussed ergonomic sleep positioning to help support her hips and prevent collapse when side-lying.
By her sixth appointment, her pain had decreased further to 2–3/10, which she described as “nothing compared to before.” She shared that she had come into treatment feeling skeptical, having tried many therapies in the past without lasting relief, but was pleasantly surprised by how she improved.
By the end of her treatment series, she reported a significant and sustained reduction in pain and was genuinely excited about her progress. She is now on a maintenance schedule and returns for photobiomodulation sessions as needed.
Conclusion
This case illustrates the potential of photobiomodulation as a supportive therapy for chronic back pain—especially in individuals who have tried multiple interventions without success. While every patient’s experience is unique, consistent treatment, proper positioning, and complementary therapies can work together to create meaningful, lasting improvements. If chronic pain is impacting your daily life, photobiomodulation may be worth exploring as part of a personalized treatment plan.
Ready to Explore Photobiomodulation?
If chronic pain is impacting your daily life, you don’t have to navigate it alone.
Book a consultation or a photobiomodulation session to find out whether this therapy may be a good fit for you by clicking the link below.
~ Dr. Charmagne